Pregnancy is a time of joy and excitement, but for many women, it can also bring physical discomfort, particularly in the form of pelvic pain during pregnancy. One of the most common types of pelvic discomfort is Pelvic Girdle Pain (PGP), affecting 1 in 5 pregnant women and causing significant discomfort in the pubic bone area, hips, lower back, and even thighs.
This article will explore the causes, symptoms, and solutions for PGP in pregnancy, as well as questions like how to relieve pelvic pain during pregnancy, what is spd in pregnancy, what is pgp in pregnancy, and when does pelvic girdle pain start.
What is Pelvic Girdle Pain (PGP) in pregnancy?
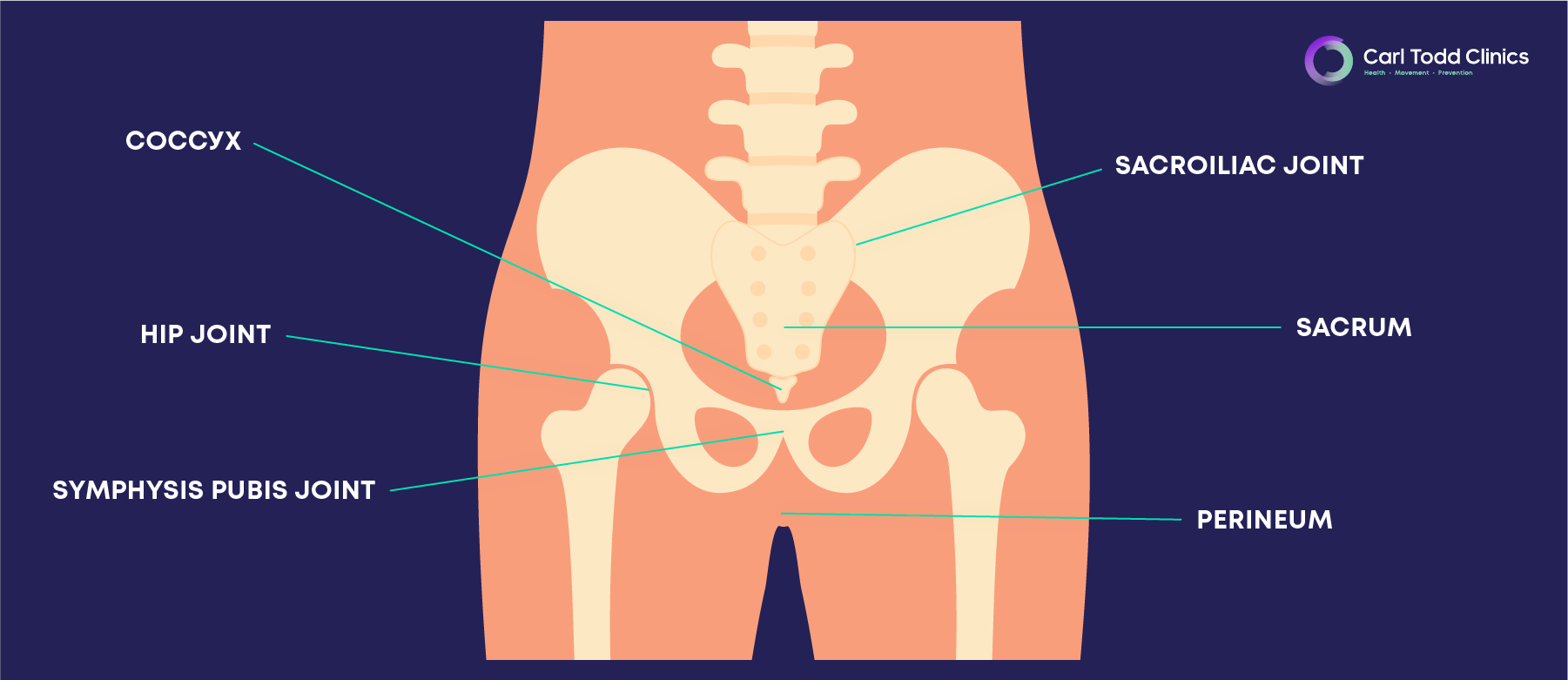
Pelvic Girdle Pain (PGP) refers to pain that occurs in the joints of the pelvis during pregnancy, particularly around the pubic bone and the sacroiliac joints (at the back of the pelvis). This condition can make everyday movements like walking, sitting, and standing uncomfortable or painful.
One specific type of PGP is Symphysis Pubis Dysfunction (SPD), which occurs when the joint at the front of the pelvis (the pubic symphysis) becomes too loose or unstable due to hormonal changes. Both SPD and PGP are common among pregnant women.
Common symptoms of Pelvic Girdle Pain
If you’re suffering from Pelvic Girdle Pain, you might experience:
- Pain in the pubic bone area, particularly where the left and right sides of the pelvis join.
- Lower back pain, often on one or both sides.
- Discomfort that radiates to the hips, groin, or thighs.
- Pain when standing on one leg, climbing stairs, or getting out of bed.
- A clicking or grinding sensation in the pelvis when moving.
These symptoms can vary in severity, ranging from mild discomfort to debilitating pain, depending on the individual and stage of pregnancy.
Why does Pelvic Girdle Pain occur during pregnancy?
During pregnancy, the body produces hormones such as relaxin, which helps soften the ligaments and joints in preparation for childbirth. While these hormonal changes are essential, they can lead to instability in the pelvic area, particularly around the pubic symphysis. The weight of the growing baby also shifts your centre of gravity, adding further strain on the pelvis and lower back.
This hormonal and mechanical change can cause the pelvic joints to move unevenly or become misaligned, leading to pelvic girdle pain.
When does Pelvic Girdle Pain start?
For many women, pelvic pain during pregnancy begins in the second or third trimester. However, for some, it can start as early as the first trimester. The pain tends to worsen as the pregnancy progresses, especially with activities that involve standing on one leg, such as climbing stairs or getting dressed.
If you’ve experienced PGP in a previous pregnancy, you may notice symptoms earlier in subsequent pregnancies.
How to relieve pelvic pain during pregnancy
Managing Pelvic Girdle Pain can require a combination of therapies and lifestyle adjustments. Here are some effective ways to relieve pelvic pain during pregnancy:
Physiotherapy: A women’s health physiotherapist can assess your condition and provide exercises designed to strengthen the pelvic floor, core, and lower back muscles. They may also use manual therapy to help realign your pelvic joints.
Osteopathy: By addressing the underlying mechanical imbalances in the body, osteopathy can relieve pressure on the pelvic girdle and reduce pain. Many women find osteopathy particularly beneficial in reducing PGP and SPD symptoms, as it promotes better posture and improves overall mobility throughout pregnancy.
Pelvic support belt: Wearing a pelvic girdle support belt can help stabilise the pelvic joints, reducing discomfort and making everyday activities easier.
Gentle exercise: Staying active with low-impact exercises like walking, swimming, or prenatal yoga can help strengthen the muscles supporting the pelvis. Exercises that focus on the core and pelvic floor are particularly beneficial for managing PGP.
Postural awareness: Good posture can help pelvic pain during pregnancy. Avoid sitting or standing for long periods and try to maintain a neutral posture, keeping your weight evenly distributed between both legs. When standing, keep your legs slightly apart and avoid crossing them when sitting.
Heat and ice: Applying heat to the lower back or pelvis can help relax muscles, while ice packs can reduce inflammation and pain in the pubic area.
Rest and avoidance: Rest is crucial, especially in the third trimester when Pelvic Girdle Pain may worsen. Avoid activities that aggravate your symptoms, such as standing on one leg or carrying heavy objects.
Sleep modifications: Sleeping with a pillow between your knees can help align the pelvis and reduce pressure on the joints. Some women find sleeping on their side with their legs bent in a fetal position more comfortable.
What is SPD in pregnancy?
Symphysis Pubis Dysfunction (SPD) is a specific type of PGP that affects the joint at the front of the pelvis, known as the pubic symphysis. The pubic symphysis is a small joint that connects the left and right sides of the pelvis. In pregnancy, this joint becomes more flexible due to the hormone relaxin, but in some cases, the extra movement can cause inflammation, instability, and pain.
SPD in pregnancy is marked by pain that worsens with activities involving separating the legs, such as walking, standing up, or getting in and out of bed. Women with SPD in pregnancy may notice:
- Pain radiating from the pubic bone to the thighs and lower abdomen.
- Difficulty with movements that involve separating the legs, such as walking, turning in bed, or climbing stairs.
- A grinding or clicking sensation in the pelvic area.
While SPD can be painful, it is manageable, and most women find relief with the right interventions.
What’s the difference between SPD and PGP in pregnancy?
Although SPD (Symphysis Pubis Dysfunction) and PGP (Pelvic Girdle Pain) are closely related, SPD refers specifically to the pubic symphysis joint at the front of the pelvis. On the other hand, PGP is a broader term that covers pain in multiple joints of the pelvis, including the sacroiliac joints at the back of the pelvis.
What causes pelvic pain during pregnancy?
The main cause of pelvic pain during pregnancy is the hormone relaxin, which helps soften the ligaments in the pelvis to prepare for childbirth. This hormone can cause the pelvic joints to become overly flexible, leading to instability and discomfort. This, combined with the additional weight and altered posture from your growing baby, puts strain on the pelvic girdle and surrounding muscles.
Other contributing factors include:
- Previous pelvic or lower back injuries.
- Overuse or repetitive movements that strain the pelvis.
- A sedentary lifestyle or excessive standing without adequate support.
Can Pelvic Girdle Pain affect labour?
Although pelvic pain during pregnancy can cause discomfort, it usually does not impact the birthing process itself. However, discussing your symptoms with your midwife or doctor is important so they can provide advice on optimal birthing positions that minimise pressure on your pelvis.
When should you seek help for Pelvic Girdle Pain?
It is important to seek medical advice if pelvic pain becomes severe or affects your ability to perform daily tasks. Your healthcare provider can assess your symptoms and recommend treatment options, which may include referral to a women’s health physiotherapist or osteopath. In some cases, imaging (such as ultrasound) may be required to rule out other conditions.
By staying active, making small adjustments to your daily activities, and following the advice of healthcare professionals, you can manage PGP and enjoy a healthier, more comfortable pregnancy.
Pelvic Girdle Pain during pregnancy is a common but usually manageable condition. Early recognition and intervention can make a significant difference in reducing pain and improving quality of life. If you’re experiencing pelvic pain, remember that help is available. Working with a qualified healthcare provider, such as a physiotherapist or osteopath specialising in pregnancy-related conditions, can provide tailored advice and relief. Book a consultation with our specialists for help managing this condition.





